When geneticist James Lee and his colleagues published a paper in June linking a gene to inflammatory bowel disease (IBD), he didn't expect the public to pay much attention. Things didn't go as planned.
“I was flooded,” he says.
By the end, Lee conducted over 25 interviews for radio shows and print media around the world and received hundreds of emails from people with IBD. “It's evidence of how common inflammatory bowel disease is,” says Lee, who works at the Francis Crick Institute in London. “And also proof of how desperate people are for better treatment methods.”
Lee's publication, published inNature, is one of several recent reports that offer hope that people with IBD may one day have better treatment options tailored to their disease. Lee and his colleagues found that changes in the activity of a gene important in the immune system could contribute to some cases of the disease. Another study found that some people with IBD produce antibodies that deactivate a crucial anti-inflammatory protein, and a third study tracked how populations of gut bacteria adapt to an inflamed environment.
The papers look at IBD from different angles, but together offer a glimpse into the possibilities that doctors could one day better match people with IBD to appropriate treatments, says David Artis, an immunologist at Weill Cornell Medicine in New York City. “Not every inflammatory bowel disease patient who comes through the door is the same,” he says. “If we can map those differences in some way, I think we can treat these people better.”
Life-altering diseases
IBD is a painful condition that results in chronic inflammation of the digestive tract. Two of the most common forms of IBD are ulcerative colitis and Crohn's disease. Both can cause diarrhea, anemia and abdominal cramps.
Like many autoimmune diseases, IBD has an unclear and complex etiology, with contributions from both genetics and environment. It is clear that the frequency of the disease is increasing in many regions of the world.
Over the past decade, researchers have compiled a long list of genetic variations linked to IBD. But Lee and his colleagues decided to examine a region of the genome where few geneticists had bothered to look: a "gene desert," what Lee called because it is devoid of recognizable genes. “We didn’t know what we would find,” he says. “And in the end we found a master regulator of inflammatory reactions.”
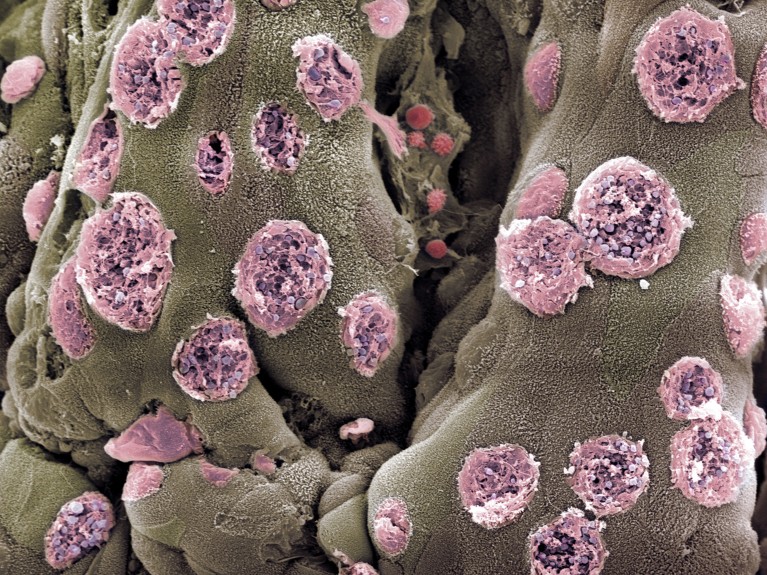
This master regulator is a piece of DNA that controls the activity of a gene called ETS2, which lies far from the gene desert. High ETS2 activity increases the ability of immune cells called macrophages to promote inflammation.
The discovery also suggested that a class of cancer drugs called MEK inhibitors could prevent activation of ETS2. The team found that these drugs could block the effects of the ETS2 protein, including the release of pro-inflammatory molecules in laboratory cells. However, MEK inhibitors can become toxic to other cells when taken long-term, Lee says, and so the team is developing ways to deliver the inhibitors only to macrophages before testing the approach in people with IBD.
Aberrant antibodies
Another study has identified a select group of people with IBD who may have a new therapeutic option in the near future. Pediatric immunologist Sophie Hambleton from Newcastle University in Newcastle upon Tyne, UK, and her colleagues analyzed samples from two children with IBD. The scientists discovered that the children produced antibodies that blocked the activity of a protein called IL-10. This protein has anti-inflammatory effects in the intestines.
But the children's antibodies meant IL-10 failed to dampen inflammation in their intestines, leading to IBD, researchers reported in JulyNew England Journal of Medicine. After the link between IL-10 and her disease was identified, one of the children was treated with antibody-reducing therapies, which relieved her symptoms.
It's unclear how many people with IBD make antibodies to their own IL-10, says Hambleton. However, when the team looked at a sample of adults with IBD, they found "a clear minority" who also produced the antibodies. “We are very confident that this will be a contribution system in more patients,” she says.
Response of the microbiome
In addition to genetics and immune cells, microorganisms are also believed to be involved in IBD. In the third study, Christopher Smillie, who studies the human microbiome at Harvard Medical School in Boston, Massachusetts, and his colleagues examined how chronic inflammation influences the evolution of microorganisms that live in the digestive tract.
They identified 140,000 bacterial strains in stool samples from people with and without IBD. Hundreds of these strains were associated with IBD, and many appear to have adapted to inflamed tissue. Among them, several could be used to predict disease severity: for example, the abundance of some strains of Eggerthella lenta decreased as levels of a protein linked to inflammation increased. The results were published in JulyCell Host & Microbepublished.
Ultimately, Smillie hopes that characterizing these microorganisms will lead to ways to monitor disease progression and classify people with IBD into groups based on how likely they would respond to potential therapies.
Each of these studies could contribute to that goal, but the work is still in its early stages, says Gabriel Nuñez, an immunologist at the University of Michigan Medical School in Ann Arbor. For example, the microbial study does not show that any of these organisms contribute to the disease, he notes. And it's unclear what percentage of people with IBD have altered ETS2 activity or produce autoantibodies against IL-10. “Maybe these are rare patients and only a handful in the world will benefit,” he says.
Still, even if just a handful of people experience relief from these results, it will be progress, he adds. “Even if you just cure one patient, it’s important to that person and their family.”

 Suche
Suche
 Mein Konto
Mein Konto

