Every other weekly visit to Seattle Children's Hospital in Washington, a five-year-old child comes in for a fresh dose of genetically modified immune cells, administered directly into the fluid around her brain.
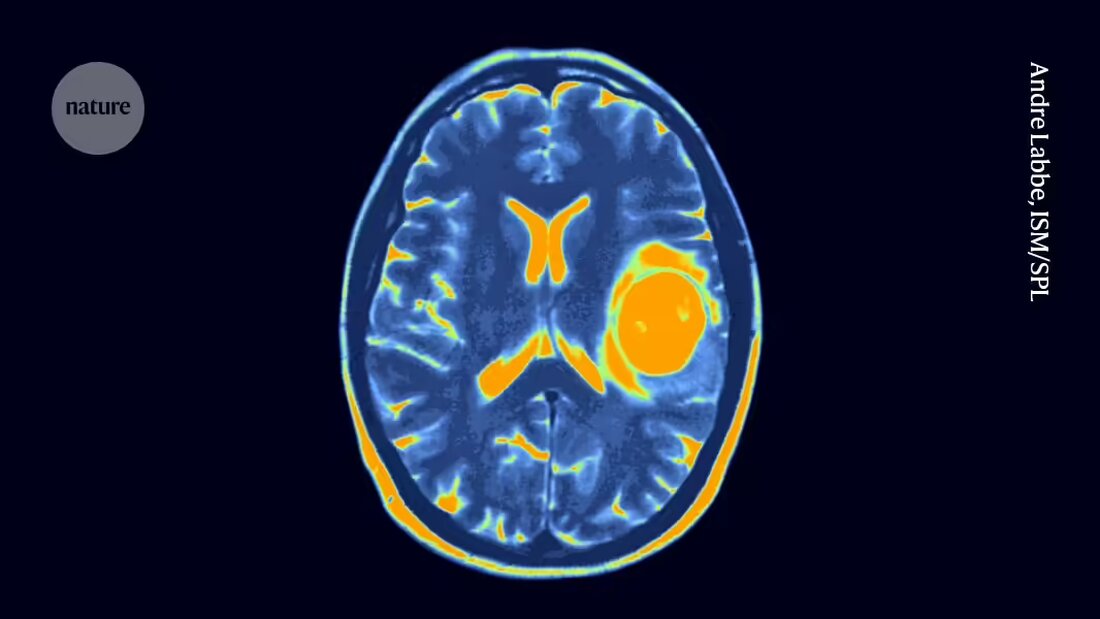
The child has been making these visits for more than three years after being diagnosed with a devastating form of brain and spinal cord cancer called diffuse midline glioma, for which there is no known cure. But the treatment, called CAR T-cell therapy, appears to have shrunk the tumor and kept it under control. With 70 treatments and counting, this five-year-old child may have received more doses of CAR T-cell therapy than anyone else on the planet.
His oncologist Nicholas Vitanza always beams when he talks about the results. Nevertheless, Vitanza is well aware that the child's reaction is unusual. Although several children in Vitzana's clinical trial may also have benefited from CAR T-cell therapy, most responses were not as dramatic or long-lasting as the five-year-old child's. The question that keeps Vitanza and others in his field up at night now is: How can they make this success less of an outlier?
On the International Symposium on Pediatric Neuro-Oncology in Philadelphia, Pennsylvania, which ended earlier this month, Vitanza and other researchers presented promising early clinical trial results that suggested CAR T cells could be an effective treatment for deadly CNS cancers in children.
The studies were designed to test the therapy's safety, not its effectiveness, and larger studies are needed to know for sure whether the treatments are beneficial. In the meantime, researchers are looking to tweak their approach to maximize their reach. “We’re seeing a glimpse of a signal,” says Jasia Mahdi, a pediatric neurologist at Texas Children’s Hospital in Houston. “Our job now is to figure out how to build on that.”
Tumor-finding T cells
CAR T-cell therapies are made up of immune cells called T cells that have been removed from the recipient and modified to produce molecules called chimeric antigen receptors (CAR) on their surface. These T cells are reintroduced to the body, where their new receptors allow them to recognize and destroy cancer cells.
Despite ongoing safety concerns The approach has proven successful in treating several blood cancers and in some cases long-lasting remissions lasting more than a decade caused. The application of CAR T-cell therapies for the treatment of solid tumors like those of the brain and lungs, however, is more demanding. Solid tumors can contain different cells with different mutations and different sensitivities to therapy. Solid tumors can also be more difficult for T cells to penetrate.
Nevertheless, studies in mice have suggested that CAR T cells may be effective against diffuse midline gliomas. New therapies for the cancer are urgently needed: Standard treatment is sometimes radiation therapy combined with chemotherapy, but the cancer is fatal and median survival is about 13 months after diagnosis, says Vitanza.
Success: a diploma
The first clinical studies on CAR-T therapy against diffuse midline gliomas in children have now been completed and the results are promising. At the meeting in Philadelphia, Vitanza presented data from a study in which 21 children with diffuse midline gliomas were treated with CAR-T cells that attack a protein called B7-H3, which is found primarily on cancer cells. Only one participant had a strong reaction to the treatment itself, and some live longer than expected, says Vitanza.
Mahdi presented data from a clinical trial of a T-cell therapy that targets a molecule called GD2. In this study, conducted at Stanford University in California, nine people with diffuse midline gliomas were treated, and the tumors shrank by more than half in four of them.
This study also had an outlier: a young man whose cancer had completely disappeared and who had remained cancer-free for more than 30 months after his first treatment. During this time he has completed high school and is now thriving at university. “All these normal things mean so much more in this context,” says Mahdi. “This reality would not have been his otherwise.”
A menu of options
Researchers are eager to extend these dramatic responses to more of their study participants. Vitzana's team has launched another study testing CAR T cells that attack four different molecules found primarily on brain and spinal cord tumors, in the hope that T cells that recognize multiple targets will be more effective.
Another team at the University of California, San Francisco, is testing CAR-T cells that express the cancer-killing receptor only when the cells are in the central nervous system. The hope is that the T cells will only be active where they are needed, making them less vulnerable to getting through "Exhaustion" becoming dysfunctional, a phenomenon known to limit the effectiveness of T cell therapies, says Hideho Okada, who researches immunotherapies and is the project's principal investigator. The team treated its first study participant, an adult with an aggressive brain tumor called glioblastoma, in June and plans to start a similar study in children.
Such modifications to CAR T-cell therapies are just the beginning, says Vitanza. Researchers are looking for further ways to optimize CAR T-cell therapies, and decades from now, doctors could be able to choose from a variety of options that can be tailored to individual patients. “It’s incredible that we’ve gotten to this point,” he says. “But in 20 years, the CAR T cells we use for patients will look very different.”

 Suche
Suche
 Mein Konto
Mein Konto