Stress can make people sick, and bacteria in the gut could, according to a study 1be to blame for mice. Research suggests that a stressed brain directly shuts down certain glands in the gut, which affects the Intestinal bacteria and the body's broader immune system.
The study is a technical masterpiece, according to neurobiologist John Cryan of University College Cork in Ireland, who reviewed the study. Most work on the gut-brain connection has focused on how bacteria affect the brain, so Cryan welcomes research into how psychological states can exert 'top-down' control over bacteria. “It’s a really cool part of the puzzle,” Cryan said. The research was conducted on August 8th inCellpublished.
Gut-brain exchange
Researchers have known for a long time that the gut and the brain “communicate” with each other. Under stress, the brain stimulates the release of hormones that cause intestinal conditions such as inflammatory bowel disease can trigger. Certain bacteria in the gut can release chemical signals that affect the brain and behavior.
However, the neural communication pathways are less understood. To find out more, neurobiologist Ivan de Araujo of the Max Planck Institute for Biological Cybernetics in Tübingen, Germany, and his colleagues focused on small organs called Brunner's glands, which are found in the walls of the small intestine. Little is known about these glands except that they produce mucus and contain numerous neurons.
De Araujo's team found that removing Brunner's glands from mice made the animals more susceptible to infection. It also increased markers for Inflammation, a flow of immune protective substances and cells that can damage tissue. The team observed a similar effect in humans: People who had tumors removed from the part of the intestine that contains Brunner's glands had higher levels of white blood cells - a marker of inflammation - than people who had tumors removed from other areas.
Bacteria in the household
A more detailed analysis showed that the removal of Brunner's glands from mice Bacteria of the genusLactobacillus eliminated that live in the small intestine. Stimulate in a healthy gastrointestinal tractLactobacillithe production of proteins that act like mortar between the cells of the intestine, keeping most of the intestinal contents inside while allowing certain nutrients to enter the bloodstream. But ifLactobacilliare gone, the gut becomes 'leaky' and "things that shouldn't enter the bloodstream do," says de Araujo. The immune system attacks these foreign molecules, causing the inflammation and disease in mice without Brunner's glands.
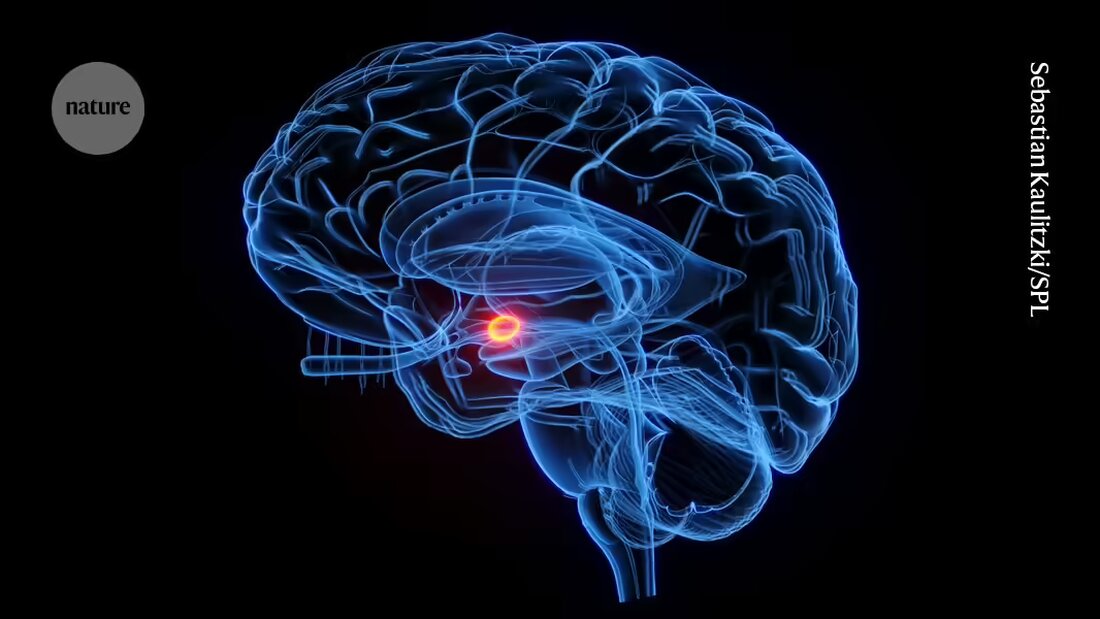
The researchers then examined the neurons of the glands. They found that the neurons are connected to fibers in the vagus nerve, a communication pathway between the gut and the brain. These fibers lead directly to the amygdala nucleus of the brain, which is involved in emotions and stress responses.
Putting mice with intact Brunner's glands under chronic stress had the same effect as removing the glands: TheLactobacillus-Values fell and inflammation increased. This suggested that the stress shut down the Brunner glands.
Communication channels
Asya Rolls, neuroimmunologist at the Technion – Israel Institute of Technology in Haifa, is impressed by the direct connection between the brain, Brunner glands, bacteria and the immune system. “The specificity of the connection is amazing,” she says. However, she cautions that the pathways in mice are not necessarily identical to those in humans.
“This paper is pretty inspiring,” says Christoph Thaiss, a microbiologist and neurobiologist at the University of Pennsylvania in Philadelphia. Understanding the specific pathways that connect the brain and gut could help researchers investigate questions such as why some people are more resilient to stress than others.
De Araujo says the study could have implications for the treatment of stress-related disorders such as inflammatory bowel disease. His group is now studying whether chronic stress affects this pathway in infants who have theirLactobacillusobtained through breast milk. “We are excited about the idea that these glands are important for normal development and immune function in early life,” says de Araujo.

 Suche
Suche
 Mein Konto
Mein Konto